Alzheimer’s Disease
What is Alzheimer’s Disease?
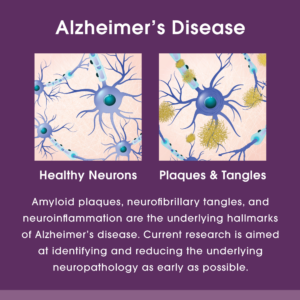
Alzheimer’s disease is a form of dementia that affects memory, thinking, and behavior. In Alzheimer’s disease, plaques of protein (amyloid) and tangles of protein (tau) accumulate in the brain, affecting its ability to properly function, resulting in cognitive impairment. While having some degree of plaques and tangles in the brain is not uncommon in the general population, those suffering from Alzheimer’s often have many more.
Younger-Onset Alzheimer’s
Although the term, early-onset Alzheimer’s disease is often used, according to the Alzheimer’s Association, the correct term for experiencing symptoms prior to age 65 is younger-onset Alzheimer’s. While most people are diagnosed after the age of 65, some may show signs of the disease before then.
With younger-onset Alzheimer’s, people can be in the early, middle, or late stage of the disease. Plaques and tangles begin forming many years, even decades, before symptoms appear. For example, if a person develops symptoms in their 70s, they likely already had Alzheimer’s disease in their 50s and 60s.
Symptoms of younger-onset Alzheimer’s disease are sporadic for the majority of sufferers. It is not attributed to genetics and its cause is unknown. As such, many younger adults are believed to be living with undiagnosed Alzheimer’s; therefore, an assessment is recommended beginning at age 50. Knowing the signs and symptoms to watch for is important, regardless of age.
Early-onset Familial Alzheimer’s Disease
In contrast to younger-onset, early-onset familial Alzheimer’s disease is determined by genetics. This rare form of Alzheimer’s disease represents less than five percent of all cases, with some research statistics indicating only one percent. It is carried on specific genes, and if a person is a carrier, there is 100 percent certainty they will develop the disease. Symptoms appear at a very young age, usually in the 30s. By mid-life, these individuals are likely to have fully developed symptoms of Alzheimer’s.
Contact Us (home page)
What is the Difference Between Alzheimer’s and Dementia?
Alzheimer’s disease and dementia are not the same thing. Dementia is a broader term for a decline in cognition that is significant enough to interfere with daily functioning.
Alzheimer’s disease is a specific type of dementia, and the most common, accounting for 60 to 80 percent of all dementia cases. There are other forms of dementia in addition to Alzheimer’s disease, and obtaining an accurate diagnosis is important for treatment and care planning.
What Causes Alzheimer’s?
While a single cause of Alzheimer’s disease has not been discovered, experts have identified modifiable (able to change) and non-modifiable (not able to change) risk factors. Non-modifiable risk factors include genetics, family history, and age. If a person has one or more of these risk factors, it does not mean he or she will develop Alzheimer’s disease, but it will be more important to talk with a doctor about checking for early signs and getting annual memory screenings in order to start proper treatment and care.
Modifiable risk factors include lifestyle circumstances, such as diet, exercise, stress level, sleep, cognitive and social engagement, and education level. These factors are considered to be among the most promising for helping to delay, moderate, or possibly prevent the onset of Alzheimer’s disease and dementia. At The CRCNJ, we offer a Psychoeducational Series that empowers patients and families with the information, support, and possible interventions for moderating brain health through modifiable risk factors.
Symptoms of Alzheimer’s
Everyone experiences changes in their memory over their lifetime, with more decline occurring in older age, but Alzheimer’s disease is different from normal age-related changes and can include some of the following symptoms:
- Memory loss that affects daily life
- Withdrawing from conversations or social situations
- Trouble with visual and spatial recognition
- Feeling confused
- Difficulty completing familiar tasks, planning, and problem solving
- Frequently misplacing items
- Changes in mood or personality
If you are experiencing one or more of these symptoms, contact The CRCNJ to determine if you are eligible for a memory screening at no cost to you.
How is Alzheimer’s Diagnosed?
Doctors use a diverse combination of tools and methods to determine if a person having memory problems may have Alzheimer’s disease. In order to diagnose a patient, a doctor may:
- Ask the patient, family members, or friends questions about the patient’s overall health, including the use of medications, past medical problems, diet, the ability to carry out normal daily activities, and changes in personality or behavior
- Conduct an evaluation that includes an assessment of memory, problem solving, attention, and language
- Review standard laboratory measures, such as urine and blood tests, to attempt to identify other possible causes of symptoms
- Perform brain scans with the use of magnetic resonance imaging (MRI), computed tomography (CT), or positron emission tomography (PET) scans. (The neurological hallmark of Alzheimer’s disease is the formation of plaques and tangles in the brain, which can appear only on specialized amyloid or tau PET scans.)
- The best way for people to gain access to specialized scans is through participation in a research study that utilizes these scans. The scans are conducted at no cost to the participant, as they are covered by the sponsor of the trial.
- Obtain a biological marker for Alzheimer’s disease through cerebrospinal fluid (CSF), retrieved via a lumbar puncture.
- This is used in research. Also, clinicians can send CSF to specialized labs for analysis.
Additionally, blood biomarkers are being actively studied and used in current research to determine if a blood test can eventually be used as a measure of plaque/tangle formation in the brain.
Doctors may repeat these tests over time to assess changes in a person’s memory or other cognitive functions.
Stages of Alzheimer’s
Alzheimer’s is a progressive disease, which means that, over time, the symptoms will gradually worsen. Experts have broken Alzheimer’s disease into seven stages:
Mild Alzheimer’s Disease
1. No symptoms emerge at this stage, but based on family history, there might be an early diagnosis
2. Forgetfulness and other early symptoms may appear
3. Reduced memory and concentration or other physical and cognitive impairments may appear
4. There is evidence of memory loss and inability to perform everyday tasks; Alzheimer’s is usually diagnosed at this stage
Moderate Alzheimer’s Disease
5. Help may be required by loved ones or caregivers
6. Impairment occurs in areas of the brain that control language, senses, reasoning, and consciousness; help may be required to get dressed, eat, or to perform other basic tasks
Severe Alzheimer’s Disease
7. Loss of speech and facial expressions appear; complete dependence on caregivers is required
As a person progresses through these stages, support from a caregiver and a professional team will become more important than ever.
Alzheimer’s Treatment
Alzheimer’s disease is a complex process and there is no cure. But there is hope that with current experimental treatments that target specific genetic, molecular, and cellular mechanisms, the underlying cause of the disease will someday be stopped or prevented. The available and prescribed FDA-approved medications for Alzheimer’s disease may help minimize symptoms of Alzheimer’s for some people for some period of time, however none are known to stop the progression of the underlying disease. These medications may help maintain functioning and may also be used to better manage behavioral symptoms. The goal is to make patients more comfortable, and caregiving easier to manage, as symptoms progress through the stages of Alzheimer's.
Path to a Cure – Clinical Trials
The acceleration of Alzheimer’s and other dementia research is critical. The only way to find a cure for Alzheimer’s disease is through clinical trials, which are research studies of medications or treatments that aim to stop the progression of the disease or reduce the symptoms. Clinical trials give participants the ability to play a more active role in their own healthcare, access to cutting-edge technology, routine monitoring, and evaluation by a team of specialists. Participation is at no cost to participants and can help others by contributing to medical research. For more information on clinical trials being conducted at The CRCNJ, please click here.
Contact us to make an appointment or call 973-850-4622 to learn more about how The CRCNJ can help.
Please click here to read,
from the Alzheimer’s Association.